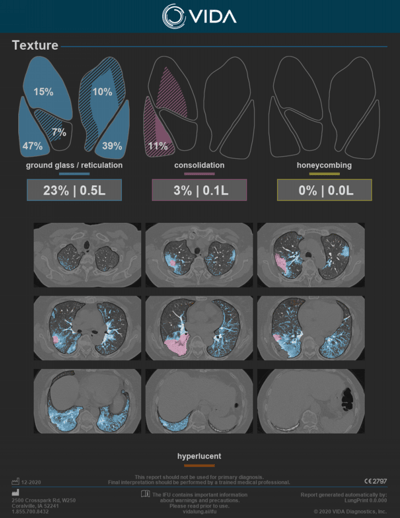
Texture Analysis Now Included in VIDA InsightsTM
COVID-19 & ILD Challenges
 Predicting progression and mortality risk to inform treatment decisions - when to be aggressive with therapy?
Predicting progression and mortality risk to inform treatment decisions - when to be aggressive with therapy?
 Understanding comorbidity to get a complete patient picture - patients with COPD have a 5.9 fold higher risk of COVID progression.1
Understanding comorbidity to get a complete patient picture - patients with COPD have a 5.9 fold higher risk of COVID progression.1
 Understanding complications and long lasting effects in recovering patients - who is at risk of readmission and why is recovery stalling?
Understanding complications and long lasting effects in recovering patients - who is at risk of readmission and why is recovery stalling?
 Identifying ILD patients early - 73% of patients have an 1+ year diagnostic delay.2
Identifying ILD patients early - 73% of patients have an 1+ year diagnostic delay.2

Getting an accurate ILD diagnosis - 55% of patients are initially misdiagnosed.3
 Assessing progression objectively - Subjective measures of progression may limit care decisions.
Assessing progression objectively - Subjective measures of progression may limit care decisions.
Availability
VIDA Insights is clinically cleared in the US, EU, Australia & Canada. Texture and Subpleura View are available in the US and Canada under the public health emergency and available for research use in the EU and Australia.
VIDA's Texture Analysis empowers physicians to address these challenges
Texture Quantification
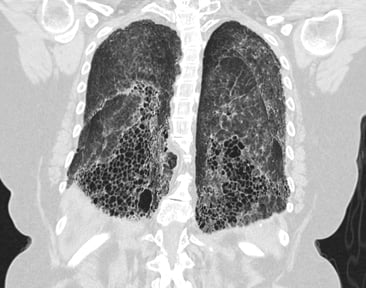
VIDA Insights provides quantitative measures and distribution of ground glass/reticulation, consolidation and honeycombing.
An overlay of these findings is also provided together with hyperlucent tissue, indicative of emphysema.
 Published works are indicating a primary imaging feature of COVID-19 to include ground-glass opacities with or without consolidation.4,5
Published works are indicating a primary imaging feature of COVID-19 to include ground-glass opacities with or without consolidation.4,5
 Quantitative lung consolidation is associated with the occurrence of major adverse hospital events for COVID-19 patients.6
Quantitative lung consolidation is associated with the occurrence of major adverse hospital events for COVID-19 patients.6
 HCRT features frequently seen in UIP (usual interstitial pneumonia) include reticulation, honeycombing and may be seen with the concurrent presence of ground-glass opacifications.7
HCRT features frequently seen in UIP (usual interstitial pneumonia) include reticulation, honeycombing and may be seen with the concurrent presence of ground-glass opacifications.7
Texture Visualization
![]()
![]() Subpleura View provides an impactful visualization of the 1mm space below the pleura, to quickly identify the presence or absence of textures in this space. This is especially useful in ILD and COVID-19 cases where these diseases often manifest.
Subpleura View provides an impactful visualization of the 1mm space below the pleura, to quickly identify the presence or absence of textures in this space. This is especially useful in ILD and COVID-19 cases where these diseases often manifest.
Subpleura View is our latest visualization innovation, joining tMPR (topographic MPR) and others to give providers a modern way to see key imaging features. Subpleura View is patent pending.
Subpleura View, COVID-19 Case
Subpleura View with Honeycombing
Comorbid Assessment
![]() VIDA Insights also provides density analysis and tMPR visualizations, assisting providers with:
VIDA Insights also provides density analysis and tMPR visualizations, assisting providers with:
- Opportunistic screening of diseases associated with low attenuation (emphysema) or high attenuation (ILAs). These quick flags of clinically significant findings aim to improve the dismal late-diagnose statistics associated with both COPD and ILD.5,8
- Immediate global impression of the patient with tMPR, resulting in increased efficiency, often making the subtle finding obvious.
- Quantitative results, empowering precision healthcare.
"VIDA Insights reduces the stress of the read. I feel like someone is reviewing the case with me."

John Newell, MD, FACR
Radiologist
-1.png?width=400&height=518&name=MicrosoftTeams-image%20(1)-1.png)
Density Analysis, COVID-19 Case
-1.png)
-1.png)
-1.png)
tMPR Visualizations, UIP Case
VIDA Insights is clinically cleared in the US, EU, Australia & Canada. Texture and Subpleura View are available in the US and Canada under the public health emergency and available for research use in the EU and Australia.
References
1. Wang, Bolin, Ruobao Li, Zhong Lu, and Yan Huang. “Does Comorbidity Increase the Risk of Patients with COVID-19: Evidence from Meta-Analysis.” Aging 12 (April 8, 2020). https://doi.org/10.18632/aging.103000.
2. Rahman, K. K. Mujeeb, and J. K. Samaria. “Diagnostic Delay and Misdiagnosis in Interstitial Lung Disease(ILD) at Primary Health Care Level.” European Respiratory Journal 48, no. suppl 60 (September 1, 2016). https://doi.org/10.1183/13993003.congress-2016.PA861.
3. Cosgrove, Gregory P., Pauline Bianchi, Sherry Danese, and David J. Lederer. “Barriers to Timely Diagnosis of Interstitial Lung Disease in the Real World: The INTENSITY Survey.” BMC Pulmonary Medicine 18 (January 17, 2018). https://doi.org/10.1186/s12890-017-0560-x.
4. Colombi et al “Well-Aerated Lung on Admitting Chest CT to Predict Adverse Outcome in COVID-19 Pneumonia.” Radiology, April 17, 2020, 201433. https://doi.org/10.1148/radiol.2020201433.
5. Wang, Bolin, et al. “Does Comorbidity Increase the Risk of Patients with COVID-19: Evidence from Meta- Analysis.” Aging, vol. 12, Apr. 2020. PubMed, doi:10.18632/aging.103000
6. Sapienza, Lucas G., Karim Nasra, Vinícius F. Calsavara, Tania B. Little, Vrinda Narayana, and Eyad Abu-Isa. “Risk of In-Hospital Death Associated with Covid-19 Lung Consolidations on Chest Computed Tomography – A Novel Translational Approach Using a Radiation Oncology Contour Software.” European Journal of Radiology Open 8 (January 1, 2021): 100322. https://doi.org/10.1016/j.ejro.2021.100322.
7. Raghu, Ganesh, Martine Remy-Jardin, Jeffrey L. Myers, Luca Richeldi, Christopher J. Ryerson, David J. Lederer, Juergen Behr, et al. “Diagnosis of Idiopathic Pulmonary Fibrosis. An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline.” American Journal of Respiratory and Critical Care Medicine 198, no. 5 (September 2018): e44–68. https://doi.org/10.1164/rccm.201807-1255ST.
8. Mapel, Douglas W, Anand A Dalal, Christopher M Blanchette, Hans Petersen, and Gary T Ferguson. “Severity of COPD at Initial Spirometry-Confirmed Diagnosis: Data from Medical Charts and Administrative Claims.” International Journal of Chronic Obstructive Pulmonary Disease 6 (2011): 573–81. https://doi.org/10.2147/COPD.S16975.